Supporting those living with HIV in primary care
In Devon, HIV prevalence is low, and therefore many primary care professionals will have limited experience of caring for persons living with HIV (PLWH). On this page we have outlined some information that will help you to provide effective support to both newly-diagnosed patients and those who have lived long-term with HIV.
Separate patient information is available on the site which reviews HIV prevention measures such as pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP).

New diagnoses
Please let us know immediately of any new diagnoses and we can help – contact details are further down this page.
Receiving and managing the delivery of a positive HIV result can be daunting. Our service is available to support you with any new diagnoses including rapid referral in to your local clinic for assessment, discussion and confirmation of the result.

Status disclosure
Sadly, PLWH still experience stigma in their daily lives and in some healthcare settings – and therefore some choose not to disclose their status widely, or at all. This is their right. However, we do strongly encourage those we look after to disclose to their GP for safety reasons (e.g. drug interactions, awareness of appropriate differentials)
Please always take care with information about someone’s HIV status and only share it with other colleagues, via referrals etc., if you have sought their consent to do so
Drug Interactions
These can make Anti-retroviral (ARV) or co-prescribed therapies less effective and/or increase drug levels and side effects.
- ARV interactions with certain statins, steroids, PPIs and multivitamins are well recognised and can be catastrophic
- Check www.hiv-druginteractions.org before prescribing or recommending over-the counter treatments
This website is a user-friendly and constantly updated resource. Any potentially concerning interactions (yellow, orange, red) can be discussed or clarified by contacting your local service. Entering prescribed HIV therapy on to your electronic systems can also help to reduce the risk of interactions via built-in interaction checkers.
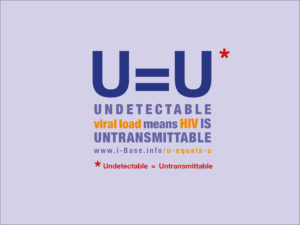
U=U
Stands for Undetectable = Untransmittable and means that people who don’t have detectable virus in their bloodstream can’t pass on HIV to their sexual partners
This is one of the most significant statements in the history of HIV research. It is based on large and well conducted observational cohort studies and is central to providing holistic and positive sexual health advice for PLWH. In the long-term we would also aspire that the statement also drives a reduction in HIV-associated stigma.
Testing
Effective and well-tolerated HIV therapy now gives PLWH a life expectancy equivalent to a matched person who is HIV negative, especially if diagnosed at an early stage of the condition. Unfortunately, many in England are still diagnosed late (CD4 <350, 43% in 2018, with the figure higher in Devon). This leads to an excess of mortality and morbidity in these patients.
- Routinely offer an HIV test to all patients requesting sexual health screen, whether or not you perceive there to be risk
- Offer HIV testing to anyone with an ‘indicator condition’, see https://www.bhiva.org/HIV-testing-guidelines
Patients within known at-risk groups for undiagnosed HIV can access postal testing for HIV. Further information on this can be found here.
HIV Testing in Torbay:
Torbay is currently classified as an area of high HIV prevalence, with >2 per 1000 PLWH in the local area (the exact figure is 2.06 per 1000 adults). Current NICE guidance recommends more frequent HIV testing in high prevalence areas. A simple first step is to recommend an HIV test to all new registrants at your surgery. More information can be found in NICE Guidance NG60.
Asking for help
Patient information pages on this site inform on how PLWH can access and seek advice from our service. The contact details listed (as below) are also applicable to clinicians seeking advice or wishing to refer or discuss any HIV queries or concerns:
Exeter: Telephone – 01392 284966
Barnstaple: Telephone – 01271 341562
Torbay: Telephone – 01803 656500