HPV vaccine: a real success story
posted by: Jonathan Shaw
What is HPV?
Human Papilloma Virus (HPV) is a common virus that spreads through intimate skin to skin contact. Unless they’re immunised, most people will get an HPV infection at some point in their lives. The good news is that the majority of these HPV infections get better on their own and don’t cause any obvious symptoms. The bad news is that some HPV infections don’t get better, and can lead to cancer later in life if they aren’t detected and treated first.
There are more than 100 different types of HPV, some of which can cause minor problems such as common skin warts or veruccas. Others, around 30 types, can affect the genital area. Genital HPV infections are really common and are also highly contagious. They are spread during sex and skin-to-skin contact of the genital areas. It turns out that some types of genital HPV can cause genital warts – which is currently the second most common sexually transmitted infection (STI) in England.
What is the HPV vaccine?
In layman’s terms, the HPV vaccine works by causing your body to make antibodies that fight HPV. If an immunised person comes into contact with HPV, the antibodies in their blood will fight the virus and protect them against being infected. It usually takes several weeks after vaccination to develop protection against HPV.
HPV has been in the news recently right?
Correct. At the start of March 2019, and again at the Start of April 2019, positive news about the impact of the HPV vaccine was published. In March Australia research highlighted the dramatic impact of their HPV vaccine programme. A Guardian opinion article by one of the study’s authors predicted a cervical cancer free Australia soon. Research published in the BMJ in April showed a similar picture emerging in Scotland where cervical pre-cancer rates are predicted to fall by 85% from HPV vaccination.
But vaccines have been in the news for other more controversial reasons too…
Correct as well. Increasingly vocal anti-vaxxer groups are a common feature in the current internet age. However it is important to review, discuss and sometimes challenge those beliefs. In 2017 a Japanese doctor won an International Prize for trying to counter misinformation which had led to massive falls in their HPV vaccine rates. At that time and since there has been no evidence that the HPV vaccine can cause harm, most clearly stated by the World Health Organisation in 2017.
So I should look to get the vaccine then?
We would recommend that anyone eligible for the vaccine programme should seek to access it and complete the two to three doses required. The potential benefits from the vaccine are significant and there is no current evidence of significant harm from receiving it.
Am I eligible for HPV vaccination in Devon?
The first dose of the HPV vaccine is routinely offered to school-age girls aged 12 and 13. The second dose is normally offered 6 to 12 months after the first. Girls who miss either of their HPV vaccine doses should speak to their school immunisation team or their GP surgery to discuss getting it. Girls who missed their HPV vaccination can still be vaccinated on the NHS up to their 25th birthday.
What about men and boys?
From the 2019-20 school year, it’s expected that 12- to 13-year-old boys will also become eligible for the HPV vaccine. The first dose of the HPV vaccine will be offered routinely to boys aged 12 and 13 , just as for girls. Final details on this are currently awaited
Men who have sex with men (MSM) do not benefit from the girls’ programme, and so may be left unprotected from HPV. From April 2018, MSM up to and including the age of 45 became eligible for free HPV vaccination on the NHS. This vaccine is accessed via sexual health clinics like ours.
So who can get the vaccine from Devon Sexual Health?
At present were are only providing vaccination to MSM under the age of 46 years, and to some of our HIV-positive patients.
Do I need two or three doses?
Anyone starting the vaccine above the age of 15 will require three doses of the vaccine. If you are aged 12-15 you will just need to receive two doses. This was decided based on early research into how people of different ages responded to the vaccine.

Trending Now
- Taking ‘the pill’. A different approach to make this method work best for you
- Does using contraception make you put on weight?
- Does contraception affect fertility?
- Updated blood pressure readings if you are taking combined hormonal contraception
- ALERT: Cervical smear scam text messages
- The “male contraceptive”

Get set for summer!
Heading to a festival this summer? Have safer festival fun by signing up for the Eddystone Trust free condoms for […]
Bank Holiday information
All Devon Sexual Health clinics will be closed on Monday 27th May for the Bank Holiday. When our clinics are […]
#StopItNow campaign returns this March
The Stop It Now campaign is aimed at deterring online child sexual abuse. The campaign is a project of the […]
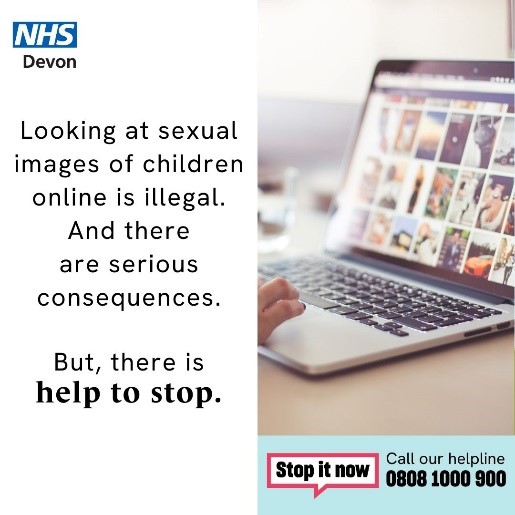
New time for Exeter Young Person clinic.
From 4 March, the Young Person drop-in clinic at Devon Sexual Health will be held every Tuesday from 3.30pm – […]