HPV Vaccinations
posted by: Don Leslie
Tea & Toast
This morning over breakfast, my 12 year old daughter, with the typical forward planning of a near-teenager, shoved a form at me to sign.
“What’s this?”
“Some sort of vaccination, you need to sign it…”
“What’s it for?”
“HPV, we’re all getting it. It’s so that we don’t get sick later…”
Naturally I gave her the benefit of my limited knowledge on HPV, how it’s related to genital warts and cervical cancer. She rolled her eyes. I decided to find out more. I asked our clinicians…
What is HPV?
Human Papilloma Virus (HPV) is a common virus that spreads through intimate skin to skin contact. Unless they’re immunised, most people will get an HPV infection at some point in their lives. The good news is that the majority of these HPV infections get better on their own and don’t cause any obvious symptoms. The bad news is that some HPV infections don’t get better, and can lead to cancer later in life if they aren’t detected and treated first.
There are more than 100 different types of HPV, some of which can cause minor problems such as common skin warts or veruccas. Others, around 30 types, can affect the genital area. Genital HPV infections are really common and are also highly contagious. They are spread during sex and skin-to-skin contact of the genital areas. It turns out that some types of genital HPV can cause genital warts – which is currently the second most common sexually transmitted infection (STI) in England.
So why is my 12 year old daughter being vaccinated for HPV?
My daughter may act like a 16 year old, but she’s 12 and is not sexually active (as far as I know). So why is she being vaccinated for HPV?
Jack, consultant in sexual health and HIV at our Exeter clinic explained it to me “As well as genital warts, some (other) types of genital HPV can also lead to abnormal tissue growth and other changes to cells within the cervix and unfortunately this can sometimes lead to cervical cancer.”
How likely is this to happen? Well, Cancer Research UK reports that there are around 3,200 new cervical cancer cases in the UK every year, that’s nearly 9 every day! Also incidence rates for cervical cancer are projected to rise by 43% in the UK between now and 2035.
Girls aged 12-13 are offered a vaccination against HPV to help protect them against the types of HPV that can cause cervical cancer. Helpfully, this is done through the schools. To get the best protection, it’s important that two injections are given, six to 12 months apart and ideally before they start having any sexual contact, which explains starting with 12 year olds in Year 7. This also gives a decent amount of time for immunity to build up.
How does the HPV Vaccine Work?
In layman’s terms, the HPV vaccine works by causing your body to make antibodies that fight HPV. If an immunised person comes into contact with HPV, the antibodies in their blood will fight the virus and protect them against being infected. It usually takes several weeks after vaccination to develop protection against HPV.
It’s worth saying here and now that the vaccine cannot cause HPV infection or cancer.
How well does the HPV vaccine work?
In Australia the federal government has been providing the vaccine for free to girls aged 12-13 years since 2007 and the HPV rate among women aged 18 to 24 dropped from 22.7% (2005) to 1.1% (2015). Since 2013 Australia has also offered the vaccine to boys, and aims to be the first country in the world to eradicate cervical cancer.
If immunised, will girls still need to have cervical smear tests when they are older?
Yes. Regular cervical screening is still needed following HPV immunisation. The NHS Cervical Screening Programme invites all women from the age of 25 to 64 to attend cervical screening. Women aged 25 to 49 are offered screening every 3 years and those aged 50 to 64 are offered screening every 5 years.
Can genital HPV infection be prevented in other ways?
Using condoms can reduce your risk of getting an HPV infection. However, condoms don’t offer complete protection. HPV can be present all over the area around your genitals and anus, and is spread through skin-to-skin contact of the genital area – not just penetrative sex. The best way to be absolutely certain, for girls, is to have the HPV vaccination.
So there we have it, teen-aged daughters can be immunised against HPV to help prevent genital warts and, more importantly, Cervical cancer. They can be advised about condom use and the risks of unprotected sex. They can’t be immunised against rolling their eyes, sighing thunderously or slamming doors, some things just have to run their course…
Blogged by:
Don. Don is a writer and father based in Devon.

Get set for summer!
Heading to a festival this summer? Have safer festival fun by signing up for the Eddystone Trust free condoms for […]
Bank Holiday information
All Devon Sexual Health clinics will be closed on Monday 27th May for the Bank Holiday. When our clinics are […]
#StopItNow campaign returns this March
The Stop It Now campaign is aimed at deterring online child sexual abuse. The campaign is a project of the […]
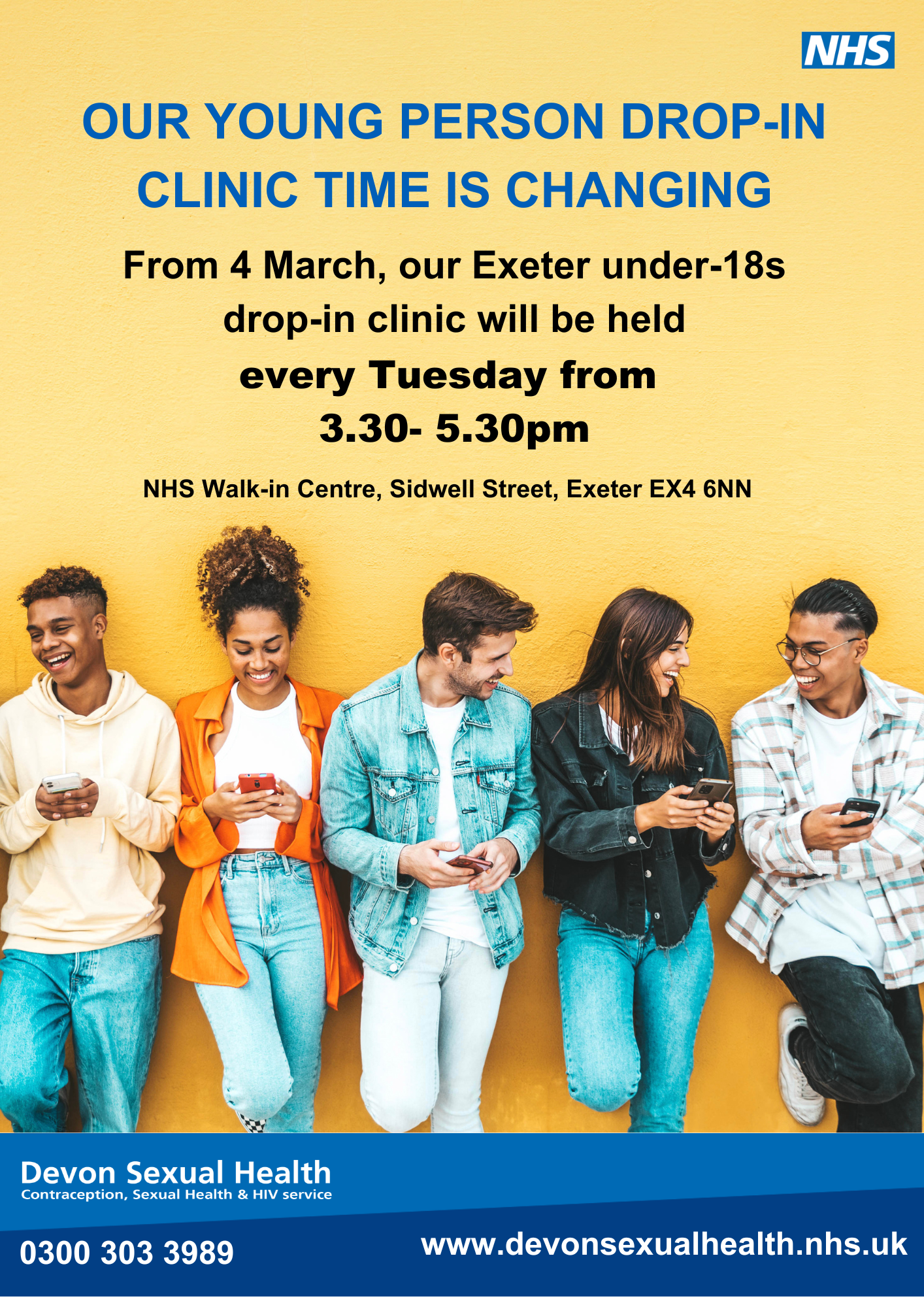
New time for Exeter Young Person clinic.
From 4 March, the Young Person drop-in clinic at Devon Sexual Health will be held every Tuesday from 3.30pm – […]